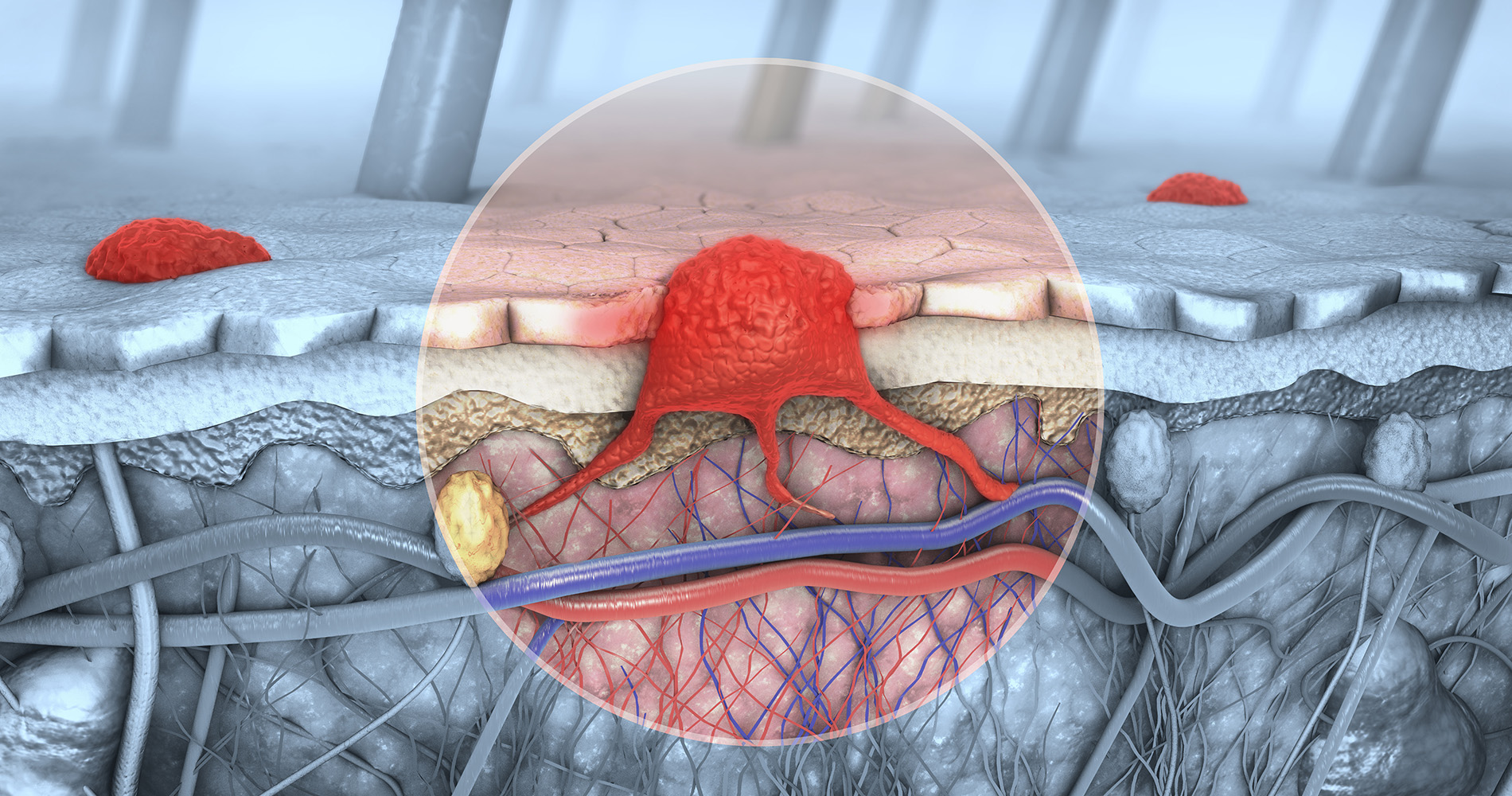
Melanoma Brain Metastases: CyberKnife Known as Radiosurgery Appears to Enhance Immunotherapy Effects When Treating Brain Tumors Caused by Skin Cancer
The combination is particularly effective for patients receiving PD-1 inhibitors
By: Mark L. Fuerst, MedPage Today
Radiosurgery was effective for melanoma patients with brain metastases receiving immune checkpoint inhibitors, with acceptable toxicities, according to new research.
Clinicians often treat melanoma with checkpoint inhibitors and patients who develop brain metastases commonly receive precisely targeted stereotactic radiosurgery for local control, the authors noted. Prolonged survival is observed for melanoma patients with brain metastases treated with combinations of therapies, and the reason may be an underlying synergy between these therapies.
“Our study supports that it is safe to use radiosurgery in patients receiving immune checkpoint inhibitors, and importantly we also describe excellent outcomes for patients with this combination of therapies, especially those who were treated with PD-1 inhibitors,” Tyler Robin, MD, PhD, of the University of Colorado Cancer Center Anschutz Medical Campus, told the Reading Room.
“It is important to point out that all patients in our study received radiosurgery and immune checkpoint inhibitors. Our study did not compare the outcomes for patients treated with immune checkpoint inhibitors with or without radiosurgery or vice versa, and so it remains possible that our findings are not the result of a synergy between these two therapies. However, the promising outcomes seen in our study, especially in patients receiving PD-1 inhibitors, lead to the hypothesis that while PD-1 inhibitors alone are active against brain metastases, radiosurgery might enhance their efficacy.”
For the study, Robin and colleagues retrospectively identified all consecutive cases of newly diagnosed melanoma brain metastases treated with Gamma Knife radiosurgery at their institution between 2012 and 2017. Included were 38 patients who had initiated checkpoint inhibitor immunotherapy within 8 weeks before or after radiosurgery.
After a median follow-up of 31.6 months, the 2-year local control rate was 92%. The median time to out-of-field central nervous system (CNS) progression was 8.4 months and 7.9 months to extra-CNS progression. Median progression-free survival (PFS) was 3.4 months, and median overall survival (OS) was not reached.
Two-thirds of patients (n=25) received anti-cytotoxic T-lymphocyte associated protein 4 (CTLA4) and one-third (13 patients) received anti-PD-1 with or without anti-CTLA4. Patients who received anti-PD-1 therapy had significant improvements in time to out-of-field CNS progression, extra-CNS progression, and PFS as compared with those who receive anti-CTLA4 therapy.
While the study did not report on the mechanisms underlying a potential advantage to anti-PD-1 and radiosurgery compared with anti-CTLA4 and radiosurgery, preclinical data from other groups have demonstrated that radiation can upregulate PD-L1, synergizing with therapies targeting this pathway, he said.
“Our study was limited to patients with melanoma, which commonly metastasizes to the brain, and immune checkpoint inhibitors have comparatively good efficacy in this disease. We are interested in studying this paradigm in other cancer types that respond well to immune checkpoint inhibitors and metastasize to the brain.”
Looking forward, the researchers said, they plan to focus on developing prospective studies aimed at defining the optimal timing and sequencing to combine radiosurgery with immune checkpoint inhibition.
Ipilimumab + Radiosurgery
Another research team noted that the anti-CTLA4 agent ipilimumab was the first checkpoint inhibitor to demonstrate a survival benefit in patients with metastatic melanoma, with an estimated medial survival of 6 months after initiation of ipilimumab alone for brain metastasis. The group’s recent open-label, multicenter, phase II study evaluated the efficacy of one administration of ipilimumab at 10 mg/kg followed by stereotactic radiosurgery and maintenance ipilimumab in a cohort of 57 melanoma patients, median age of 54, with brain metastases.
Median survival time was 13.2 months — longer than the median survival time of 5.6 months in the reference population. The disease control rate was 49%.
The most serious treatment-related adverse events were colitis (10.5%), hepatitis (10.5%), hypophisitis (8.8%), and headache (8.8%); one patient developed radionecrosis.
“High-dose ipilimumab combined with stereotactic radiosurgery provides a rather good OS in melanoma patients with brain metastases, with the usual manageable safety profile of ipilimumab,” wrote Laurent Mortier, MD of the University of Lille in France, and colleagues. “Whether this result is simply due to the addition of local control of the immediate neurological risk of stereotactic radiosurgery and the systemic effect of ipilimumab or to a real synergistic effect of radio-immunotherapy remains unclear.”
Treatment-related Injury
Immunotherapy-treated melanoma patients with brain metastases who receive stereotactic radiosurgery may have higher rates of treatment-related injury, including radiation necrosis, which can be difficult to differentiate from disease progression.
In another study, a cohort of 104 melanoma patients with brain metastases who received stereotactic radiosurgery or stereotactic body radiation therapy and immunotherapy was compared with a group of 29 patients who had not received radiosurgery to examine characteristic radiographic findings to guide decision-making.
Among the immunotherapy group, the treatment appeared to be effective in 16 patients (15.4%). Of the 29 who did not receive immunotherapy, only one had a pathologically confirmed treatment effect.
“MRI findings were consistent with existing data on radiation necrosis in glioblastoma multiforme, which could help guide decision making in melanoma brain metastases, although perfusion data for clear tumor progression was limited,” stated the researchers, led by Justin L. Sovich, MD, of the University of Texas MD Anderson Cancer Center.
Here is the link to the study results:
To learn more talk to our cancer experts at the CyberKnife Center of Miami 305-279-2900